Can the healthy brain offer clues to curing Alzheimer’s?

“Have you cured Alzheimer’s disease yet?”
This is a common question people ask when they discover that I do brain and memory research. And I can understand why. Many of us have witnessed elderly people spending their final years unable to recognize loved ones or to take care of themselves due to Alzheimer’s. It’s terrifying to imagine losing your independence in this way.
Unfortunately, despite extensive research, there are no effective treatments for Alzheimer’s disease.
Many of the promising medications that have been developed have had disappointing results in clinical trials, possibly because those enrolled have already had Alzheimer’s for too long.
The brain changes caused by Alzheimer’s actually start many years, even decades, before the onset of serious memory problems. That is why scientists like myself think it’s critical to find ways of detecting the disease before symptoms appear.
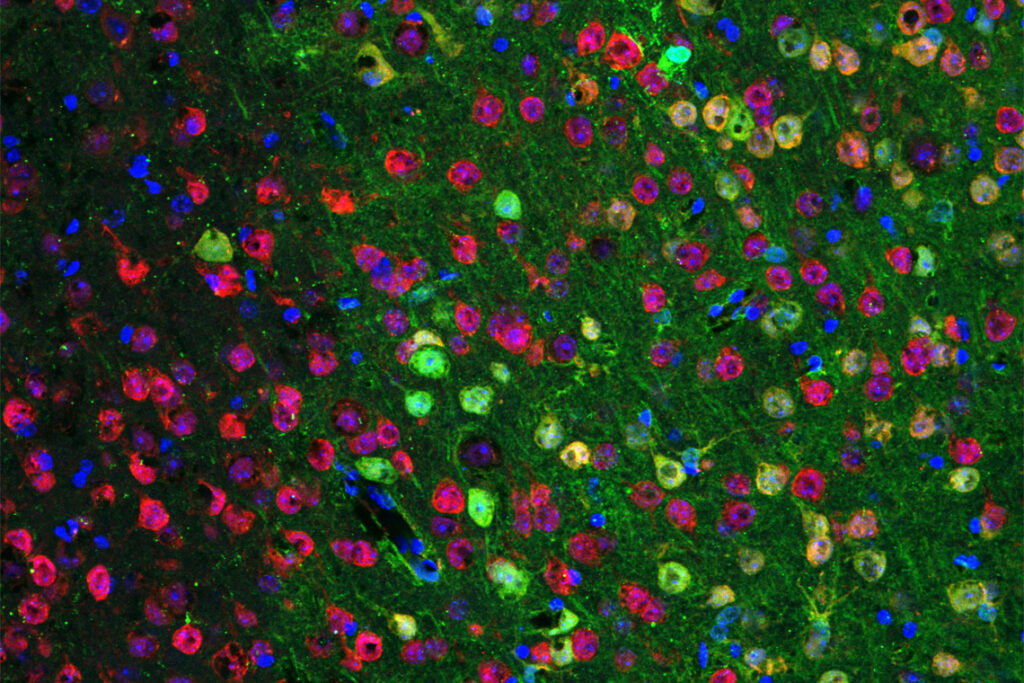
I study the “memory centres” of the brain at the Rotman Research Institute at Baycrest Health Sciences and as an assistant professor at the University of Toronto. These memory centres are the first to “shrink” – in other words, lose brain tissue – due to the buildup of proteins that cause Alzheimer’s disease.
I recently published a study that used magnetic resonance imaging (MRI) to measure the region of the brain that we think develops those disease-causing proteins before any other brain region.
Measuring the brain
This study was the first to measure the size of a specific area within the brain known as the anterolateral entorhinal cortex.
Many previous studies have examined brain tissue or the volume of the hippocampus, which is a closely related region. However, we think the hippocampus is affected later in the disease compared to the anterolateral entorhinal cortex.
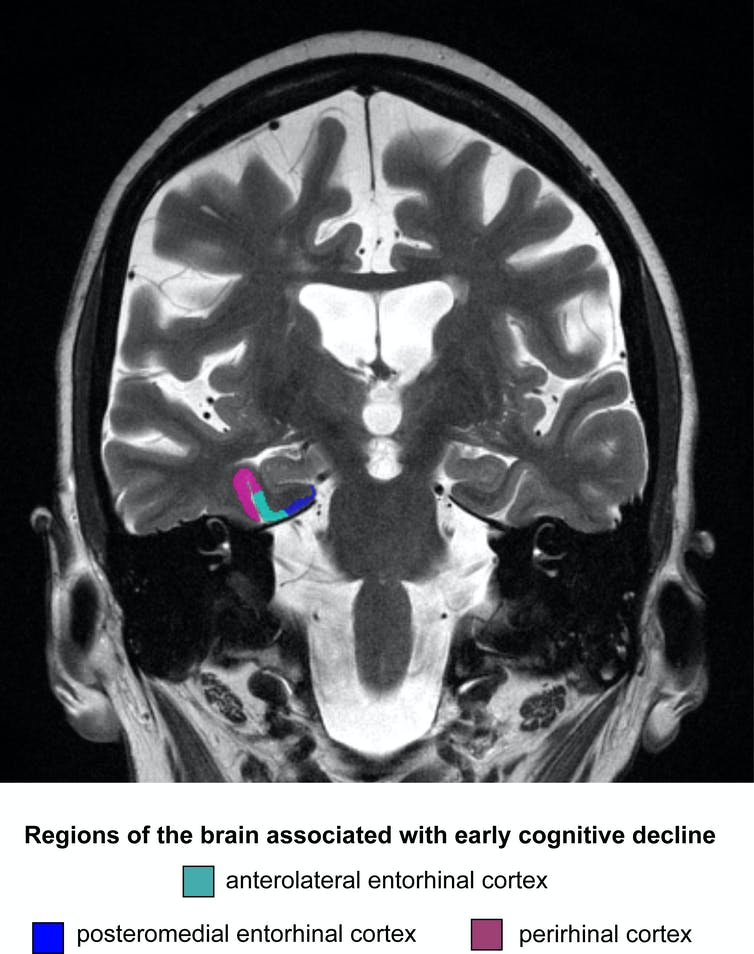
Our study was also the first published paper to show that older adults with very subtle memory problems (not yet noticeable in their everyday lives) have less brain tissue in the anterolateral entorhinal cortex.
The research my laboratory conducts on structural (brain size) biomarkers of Alzheimer’s disease is directly related to the development of tools to diagnose and evaluate treatments for neuro-degenerative disease.
It’s extremely important to me and my colleagues that our science will some day help someone with dementia suffer less, or develop the disease more slowly.
How memories are stored
While a large part of my research program is dedicated to identifying tools to identify Alzheimer’s disease, another focus of my laboratory is on the basic “cognitive neuroscience” of memory.
The goal is to understand how memory works in the absence of a neuro-degenerative disease (in other words, to figure out how memory works in healthy people).
For example, there are still competing theories about the types of mental activities that the anterolateral entorhinal cortex supports. Some of my research is focused on understanding exactly which mental activities involve this critical region.
While we have made considerable progress over the past half-century or so in understanding how the brain supports our ability to remember, there is still much to learn.
The tools and data analytic techniques are getting better and better, and these advances are allowing my team to make exciting new discoveries about how we create memories, why everybody sometimes forgets things and how we might improve our memories.
Before the brain is “broken”
This basic research on memory is crucially important in our scientific quest to help people with Alzheimer’s disease.
Only by knowing how the brain works before it is “broken” will we be in a position to develop treatments for dementia.
For example, once we know which brain networks are involved in a certain type of memory, we can help individuals with Alzheimer’s disease use different parts of the brain to compensate for the areas that are damaged.
If we can develop memory strategies or cognitive interventions that tap into the areas of the brain that are still intact, we could limit the impact of a patient’s memory impairment. In other words, a healthy brain area may able to take over some of the jobs of an impaired or shrunken brain area.
Through my research and public outreach, I try to share why it is critical to study the basic cognitive neuroscience of memory. In honour of those whom we have lost to Alzheimer’s disease and other forms of dementia, I will continue to conduct research that will, I hope, make a significant impact in our collective efforts to diagnose, treat and perhaps even cure Alzheimer’s disease.
I hope too that a better understanding of this disease, and the brain regions affected by it, will ease the fears of those who dread someday losing their most cherished memories.
Rosanna Olsen is a scientist at the Rotman Research Institute, Baycrest Health Sciences, and an assistant professor in the department of psychology at U of T.
This article was originally published on The Conversation. Read the original article.