Biology professor gets funding boost to develop new ways to test rare muscle disorder

University of Toronto Mississauga (UTM) biology professor Bryan Stewart is teaming up with a colleague to tackle a fatal pediatric disease.
Stewart and U of T assistant professor Penney Gilbert are growing tiny muscles in an effort to help those with Duchenne Muscular Dystrophy. Their project recently got a $459,000 boost via a Canadian Institutes of Health Research grant.
Until now, their research has been unfunded and, as Stewart explains, they’ve been “scraping together bits and pieces to get it going.”
Duchenne Muscular Dystrophy, or DMD, is a genetic disease that usually affects boys. The progressive neurological disorder weakens muscles in the entire body. Over time, children with DMD will develop problems walking and eventually the muscles used for breathing and the heart will give out, Stewart explains, adding those with DMD don’t typically live past their early 30s.
“It’s a very bad disease because everyone dies,” he says. “There’s no cure.”
DMD tends to affect boys because it is what’s known as an X-linked gene, which means the mutation that causes the disease is carried on the X chromosome, Stewart explains. Males only have one X chromosome, which they receive from their mother. If that chromosome carries the gene mutation, “it’s the only X chromosome the son has so he has the disease,” Stewart continues. Females, meanwhile, have two X chromosomes and would need to carry the mutation on both to have DMD. While females are carriers, it’s rare for them to have the disease.
“The underlying causes of DMD are very well known,” Stewart says. “(But) there’s really no good treatments.”
Describing himself as a “new entry into the DMD field,” Stewart explains his background is in neurobiology, studying physiology, neurons, muscles and how they work.
“My whole research program is how the neurons function and they develop,” he says. “Until this point, all my research has been on fruit flies. There are good reasons for that. Practical reasons. Scientific reasons. And that’s the system I chose to work with a long time ago.”
His collaborator, Gilbert, specializes in muscle and stem cell biology. Her research program is designed around understanding tissue engineering and using muscle stem cells to grow muscles.
“We have this complementary expertise,” Stewart says, noting they met about five years ago and discovered their research interests were aligned, deciding “let’s give it a shot.”
According to Stewart, until now, there hasn’t been an effective way to study the basic biology of DMD, in part because it’s a human disease and you “can’t just go and do experiments on people.”
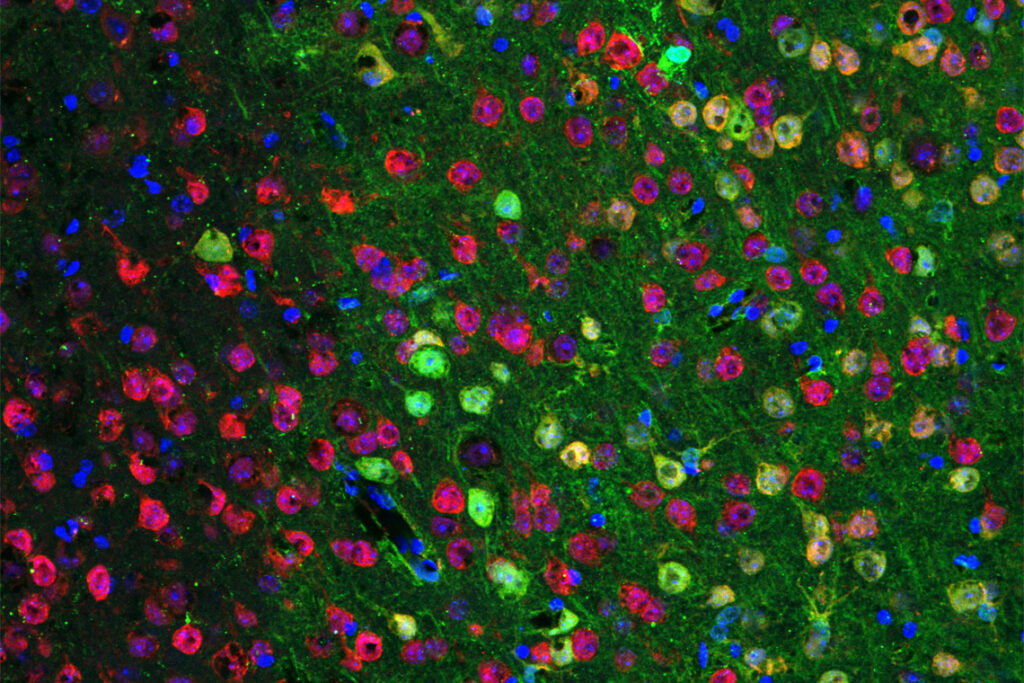
Stewart and Gilbert are creating a way to study that basic biology and test treatment options. Using techniques developed by Gilbert’s lab, and with the help of PhD student Christine Nguyen, they are using stem cells to grow tissue that looks and behaves like a muscle.
“It’s basically a miniature muscle,” Stewart says. “By studying the tissue in a 3D culture system, I think it’s a much better mimic or model of a real muscle. And now that we’ve done that, we’re at this state where we can ask questions.”
The goal of the project is to determine the effects of the mutation on the neuromuscular structure and how the basic physiology of the system is understood.
“We feel there is sufficient lack of evidence there,” Stewart says. “Once we have that and characterize that system, we can test existing therapeutics to improve the function.”
Taking off-the-shelf compounds already approved for other cases, Stewart and Gilbert are looking to find treatments that could alleviate any of the problems that are detected in Duchenne’s tissue.
Stewart cautions that their goal is not to come up with a prescriptive therapy or drug regimen, but is instead intended to fill in information about how DMD works, which could lead to an overall strategy to treat the disease.
“There’s a lot of literature about what they think is going on in the cells, so we can test all this now,” Stewart says. “We think there’s a sufficient gap in our knowledge that it’s worthwhile to check these things.”
This story first appeared in the 2020 Spring issue of M Magazine.