How does COVID-19 invade our bodies so easily? U of T researchers use ‘organ-on-a-chip’ model to find out
In order for a COVID-19 vaccine and antiviral drugs to be developed, scientists first need to understand why this virus spreads so easily and quickly, and why it invades our bodies with seemingly little resistance from our immune system.
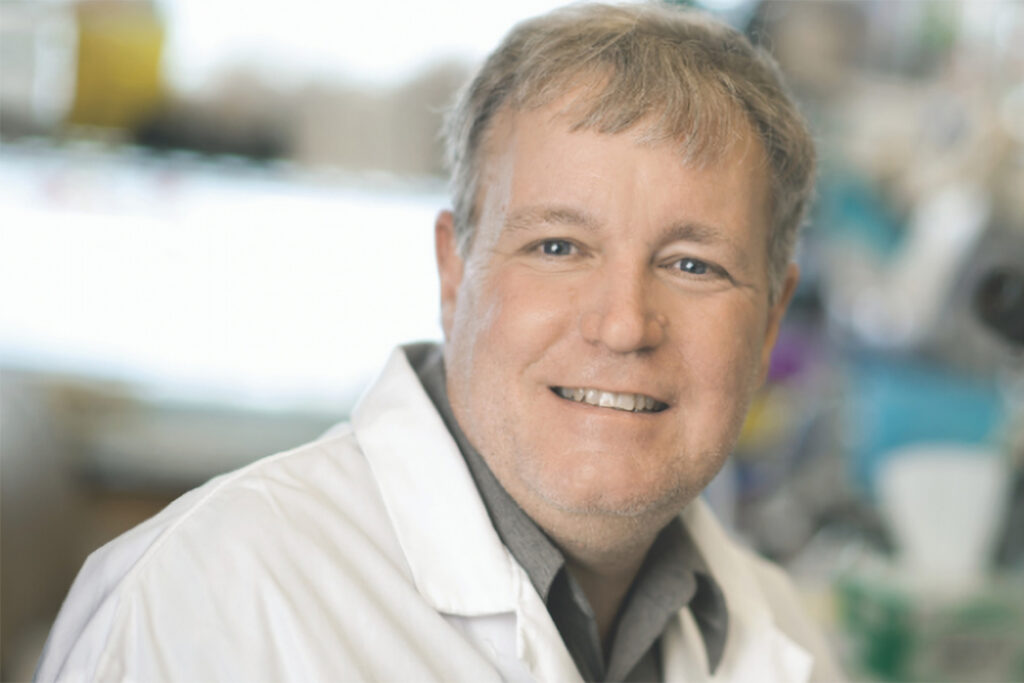
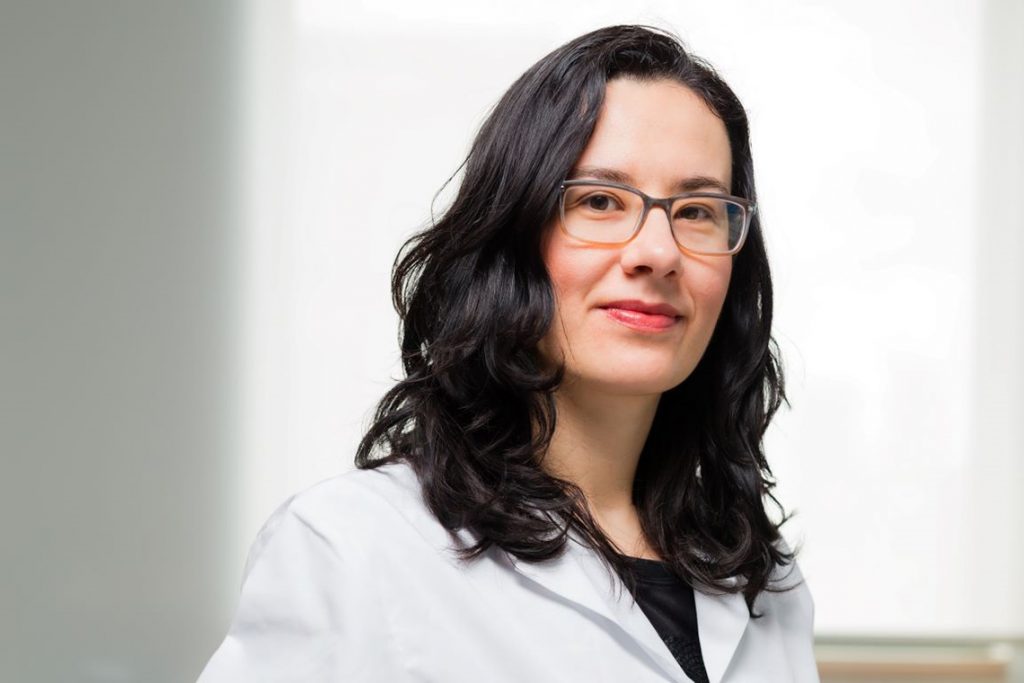
To understand how COVID-19 enters the body and does its damage, a team of top researchers from universities, hospitals and the National Research Council of Canada (NRC) at the Centre for Research and Application in Fluidic Technologies, or CRAFT (a collaborative centre between the University of Toronto and the NRC), are adapting an approach developed by U of T’s Milica Radisic, Axel Guenther and Edmond Young to create miniscule models of the nose, mouth, eyes and lungs.
The focus will be on understanding why this virus is so effective at breaking through the body’s natural defenders against viral and bacterial invaders, otherwise known as epithelial barriers. These barriers – created by epithelial cells that pack themselves tightly together – are present throughout our bodies.
“Normally, these epithelial barriers do a good job of helping us fight infections,” says Radisic, who is a professor in the department of chemical engineering and applied chemistry in the Faculty of Applied Science & Engineering.
“But this virus has found a way to invade the barriers. That’s our focus – why is this?”
In recent years, Radisic’s research has allowed her to make important progress in developing models of the heart on computer chips. The hearts – made from human cells – capture the key functions of an actual heart. That research, in turn, has been extremely effective in regenerating heart cells. Radisic has also used this organ-on-a-chip model to study how nanoparticles from air pollution damage our organs.
Now, by creating mini-models of other human organs,the researchers can take a detailed view of just how COVID-19 is working.
“This method allows us to study the problem without having to touch a human and potentially harm someone,” says Radisic, who is also Canada Research Chair in Functional Cardiovascular Tissue Engineering.
“That’s the beauty of it. We can do our research early in the viral infection. You can’t do that with a human, because once you know you have COVID-19, you’ve been infected for two weeks. With organ-on-a-chip, we can study what happens within 24 hours of COVID-19 entering the body.”
A big part of the challenge with COVID-19 is that it’s new and no one is immune.
“There isn’t anyone who has developed the T and B cells that are part of what we call ‘adaptive immunity’ – the cells you build up as you are exposed to diseases. We are all born with innate immunity. This works early when we are invaded with a virus. It finds things that don’t belong in your body and tries to clean it up.”
Radisic says having a lung-on-a-chip will enable the team to study the innate early response of the immune system to COVID-19.
Once the models are built with commercially available cell lines to set the groundwork, the human cells for the organs-on-a-chip will be supplied by CRAFT members Tereza Martinu (respirology) and Ana Konvalinka (nephrology) of University Health Network and U of T’s Faculty of Medicine. The live virus will be acquired from Karen Mossman, a researcher in pathology and molecular medicine at McMaster University. Mossman was involved in isolating the virus with U of T scientists Samira Mubareka and Robert Kozak, who are based at Sunnybrook Health Sciences Centre.
“Karen has the live virus, so we will give her the chips and she will infect the organs in a special level three facility,” Radisic says.
Other CRAFT team researchers include Teodor Veres and his colleagues Daniel Brassard, Lidija Malic and Sue Twine from the NRC; Guenther and Young, both of U of T’s Faculty of Applied Science & Engineering; and Wolfgang Kuebler of the Keenan Research Centre for Biomedical Science, St. Michael’s Hospital and surgery and physiology at U of T.
The group will also experiment with the “Powerblade,” a technology the NRC in Montreal is using to test the blood of astronauts while on space missions. It will be repurposed by the research team to examine its potential for testing people with COVID-19 when they arrive at a hospital.
“Once we figure out which molecules are biomarkers for a severe case of COVID-19, the Powerblade will be able to read that at point-of-care,” Radisic says.
“The health-care providers will then know how your innate immunity is reacting and if the virus will be severe or not. The problem with COVID-19 is that it works fast. You look good one minute and then, suddenly, you can be in real trouble. So getting earlier markers is important.”
Read about the action fund U of T launched to support high-impact COVID-19 research